By Adi Pajazetovic, DPM, Kalani Parker, DPM
Tinea pedis resistant to treatment may require systemic antifungals
History
A 67-year-old male with no known significant past medical history presented to clinic with an itchy dermatitis like lesion within his left fourth web space. Lesion has been present for an undefined length of time.
Physical Examination
Patient presented with an eczematous/tinea like lesion within the left fourth web space along with maceration to the area.
Diagnostic Testing
A shave biopsy was performed and a submission of a skin fragment measuring 0.3 x 0.3 x 0.1 cm was received to confirm diagnosis of tinea.
Histological Findings
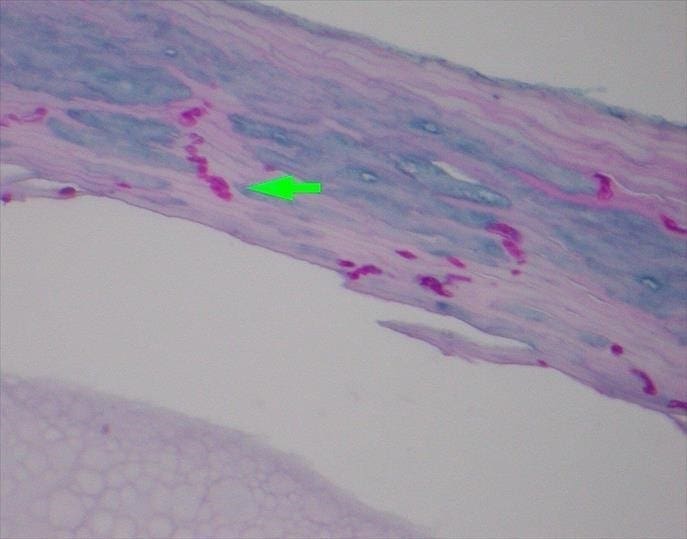
The received specimen was sectioned, and the sections demonstrated scattered neutrophils within the stratum corneum. A periodic Acid Schiff (PAS) stain test was performed, which highlighted septated fungal hyphae, morphologically consistent with dermatophytes within the keratin layer. A PAS is commonly used stain in mycoses diagnosis as it highlights the carbohydrate rich cell wall of fungi1.
Diagnosis
Dermatophytosis involving the volar or near volar skin of the foot (Tinea Pedis)
Discussion
Tinea pedis is one of the most common fungal pedal skin infections and is caused by a dermatophyte. It can present as an interdigital manifestation, moccasin patterned, or with inflammatory vesicles, and can often be associated with onychomycosis2. The condition generally affects an older population and can be as prevalent as 70% of the population .
The dermatophytes are filamentous fungi in the genera Trichophyton, Microsporum and Epidermophyton. They metabolize and subsist on keratin and infection typically is superficial involving the epidermis. The clinical features include interdigital, hyperkeratotic and vesiculobullous tinea pedis. The interdigital tinea pedis manifests as pruritic, erythematous erosions or scales between the toes, especially in the third and fourth digital interspaces3. BakoDx now offers a web space DNA test that can help differentiate the cause of the interdigital infections. Infectious agents tested include fungi such as dermatophytes and specific bacterial agents as well. The sampling is a simple shave biopsy of the interdigital lesion. All that is needed is a visible sample of tissue. This easy procedure will aid in the treatment of the infection as it specifies the inciting organism.
Treatment
Tinea pedis rarely causes significant morbidity or mortality, but there is some evidence that it can act as a portal of entry for bacteria causing bacterial cellulitis. Topical antifungal treatment is generally adequate. For extensive infections and especially involving immunocompromised patients, oral therapy may be required. Relapse from inadequate therapy is common and reinfection can reoccur in 10% of cases. Tinea pedis resistant to treatment may require systemic antifungals such as terbinafine, fluconazole, or itraconazole. In cases involving both fungal and bacterial infections, a concomitant antibiotic therapy is justified.
Most superficial cutaneous dermatophyte infections are managed with topical therapy such as azoles, Nystatin, etc. Oral treatment with terbinafine, itraconazole, fluconazole, and griseofulvin is used for recalcitrant infections. The use of combination antifungal and corticosteroids is discouraged as it is unnecessary to achieve cure and increases the risk of steroid induced skin atrophy3.
References:
1: Wang, Michael Z (02/01/2017). “Correlation between histopathologic features and likelihood of identifying superficial dermatophytosis with periodic acid Schiff-diastase staining: a cohort study”. Journal of cutaneous pathology (0303-6987), 44 (2), 152.
2: Usatine, R. P., Smith, M. A., Mayeaux, E. J., & Chumley, H. S. (2019). The color atlas and synopsis of family medicine. New York: McGraw-Hill Education.
3: Goldstein AO, Goldstein BG. Dermatophyte (tinea) infections. UpToDate, 2019.