A New Gold Standard for the Diagnosis of Small Fiber Neuropathy
What is small fiber peripheral neuropathy and when might I be expected to see it amongst my patients?
Small fiber peripheral neuropathy is a form of neuropathy that is limited to the terminal, intra-epidermal ends of sensory nerves. This expression of peripheral neuropathy commonly presents in a stocking or glove-like distribution. Those that exhibit neuropathy in this pattern, without involvement of large nerve fibers are said to have pure small fiber peripheral neuropathy. If the nerve pathology progresses proximally to involve larger nerves, the neuropathy becomes mixed. Of course diabetics can also be stricken with large fiber polyneuropathy or mononeuropathy; however, these are far less common.
The most common causes of small fiber peripheral neuropathy are diabetes mellitus (types I and II) and idiopathic cases. Additional causes include those that are related to chronic alcohol abuse, HIV infection, amyloidosis, and cases that are iatrogenic (chemotherapy).
What is epidermal nerve fiber density testing?
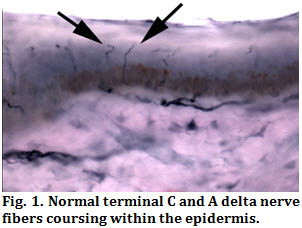
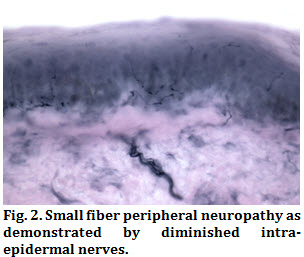
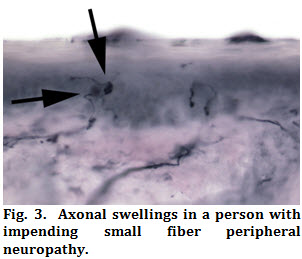
Epidermal nerve fiber density testing (ENFD) is not a new technology, in fact, this technique has been used by neurologists for roughly 15 years. This test takes advantage of the fact that most forms of peripheral neuropathy progress in a distal to proximal fashion, beginning with the most distal sensory nerve twigs (C fibers and A delta fibers), and then progressing proximally to involve nerves of larger diameter. This is why diabetic patients so often present with neuropathy in a “stocking”-like distribution. In short, epidermal nerve fiber density testing consists of the immunohistochemical analysis of a punch biopsy of skin to qualify and quantify the number unmyelinated C-fibers and myelinated A delta-fibers within the epidermis per unit area. Because the skin has a relatively uniform number (or density) of epidermal nerves at any one anatomic site, and this density is not influenced by gender or patient age, an epidermal nerve fiber density that lies below the normal bell curve is indicative of small fiber peripheral neuropathy (Figs. 1 and 2). In addition, prior to the onset of bona-fide small fiber neuropathy, there may be degenerative changes among epidermal nerves that are predictive of pending neuropathy (Fig. 3). Such degenerative changes may be seen in predisposed persons prior to the onset of clinical symptoms.
How does a punch biopsy for ENFD differ from a standard punch of skin?
From a clinical perspective, biopsies taken for ENFD are similar to those obtained for any other skin condition with a few exceptions. Because the density of nerve fibers must be tabulated across a known surface area, the breadth of a punch biopsy taken for ENFD is standardized to a particular size.
An additional difference with biopsies taken for ENFD, involves the procedure itself. Special techniques are used to harvest the sample to avoid traumatizing the epidermal surface. Even minor trauma may make the biopsy difficult or impossible to interpret.
A final substantial difference between a routine punch biopsy and those taken for ENFD is its handling after the punch has been performed. Punches taken for ENFD cannot be placed in formalin, rather, they require special fixative. Such fixative it usually rinsed off prior to mailing, as if left in contact with the tissue for more than 24 hours, the test will be compromised.
What are the advantages of epidermal nerve fiber density?
The chief advantages of ENFD over other testing methods are as follows: 1) it is a purely objective measure of small nerve disease 2) it may predict the onset of neuropathy 3) it may be readily performed in an office setting 4) it provides a baseline so that the benefits of therapeutic agents may be measured 5) it is highly specific and sufficiently sensitive and 6) it is relatively quick and easy to perform with an exceedingly low complication rate.
How will my patients be affected?
Because epidermal nerve fiber density testing requires only a simple punch biopsy of skin, and the ideal location is proximal to the shoe-covered skin of the foot, the inherent complication rate is exceedingly low. Patients will avoid bathing for 2-5 days; however, can resume showering the day after the biopsy is performed. In most instances, sutures are unnecessary.
Does Insurance Pay for Epidermal Nerve Fiber Analysis?
Because epidermal nerve fiber analysis uses established techniques, and is well founded in research at institutions such as Johns Hopkins Medical Center, it is recognized by most insurances as a useful and potentially necessary diagnostic test. We have not seen payment denied by most large insurers.
For further questions regarding epidermal nerve fiber density analysis, contact your consulting podiatric clinician or visit us on our website at www.bakopathology.com.
References:
1) McArthur JC, Stocks EA, Hauer P, Cornblath DR, Griffin JW. Epidermal Nerve Fiber Density. Normative reference range and diagnostic efficiency. Arch Neurol 55:1513-15120, 1998.
2) Ebenezer GJ, P Hauer, C Gibbons, JC McArthur, M Polydefkis. Assessment of epidermal nerve fibers: a new diagnostic and predictive tool for peripheral neuropathy. J Neuropathol Exp Neurol 66(12):1059-1073, 2007.
3) Gibbons CH, Griffin JW, Polydefkis M et al. The utility of skin biopsy for prediction of progression in suspected small fiber peripheral neuropathy. Neurology 66:256-258, 2006.