By Morgan Baxter, DPM, Aron Block, DPM, Lillian Youhkana, DPM
Blastomycosis is a type of fungal infection that can be acquired from inhaling fungal spores
History
A 53 year old healthy male presents to clinic with concerns of a rash involving raised bumps for about a month. He thought it was a cluster of warts, but has not had any relief with over the counter topical medications. He does mention that about a month ago, he was raking leaves barefoot. The bumps are not painful but have started to leak and have not gone away. He resides in Ohio near Lake Erie.
A punch biopsy of a representative lesion was submitted.
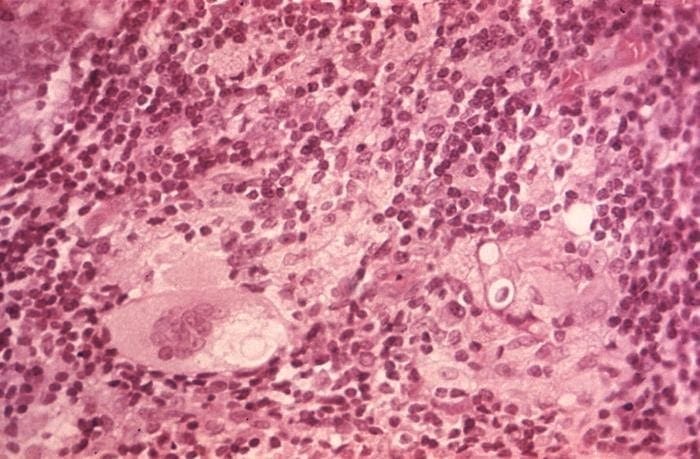
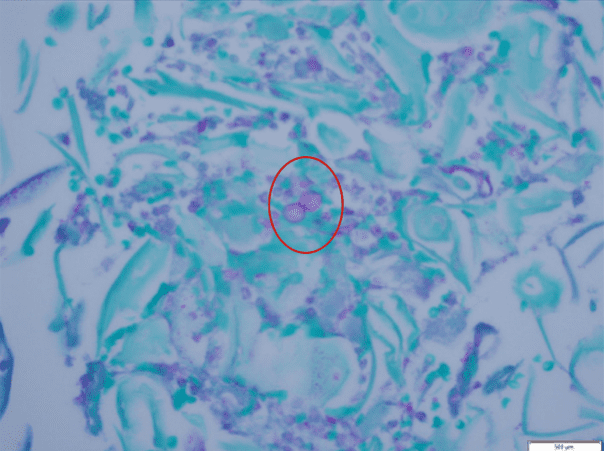
Histologic findings:
Diagnosis
Blastomycosis
Differential Diagnosis
Other cutaneous infections can mimic cutaneous blastomycosis including other endemic mycosis such as histoplasmosis and coccidioidomycosis. It has been found that cutaneous blastomycosis may very closely resemble pyoderma gangrenosum or keratoacantoma or malignancies such as basal cell carcinoma or squamous cell carcinoma. For proper diagnosis a skin biopsy is vital in differentiating blastomycosis infection from these other diseases.
Discussion
Blastomycosis is a type of fungal infection that can be acquired from inhaling fungal spores from the air. It is found in the United States and Canada and is concentrated in the Ohio and Mississippi river valleys and the Great Lakes region. Blastomycosis is typically found in soil and decaying organic matter. It manifests as a primary lung infection in the majority of cases. In individuals with weakened immune systems, the infection can spread to other areas of the body such as the skin. Following pneumonia, cutaneous lesions are the next most common manifestation of blastomycosis. The skin lesions are either verrucous or ulcerative. Bone, prostatic and CNS blastomycosis are also fairly common presentations of this infection. The disease is often misdiagnosed, particularly as malignancy. Search for the organism by microscopy and culture should be considered, even in those with a classic presentation of other illnesses. Most people with blastomycosis will need treatment with prescription antifungal medications. Depending on the severity of the infection, the course of treatment can range from six months to a year. Mild and moderate fungal infections involving the skin and lungs are best treated with Itraconazole. Amphotericin B should be used in severe infections involving the lungs. In conclusion, a thorough history including a geographical location is imperative to help make the accurate diagnosis of a blastomycosis infection.
References:
Chapman SW, Dismukes WE, Proia LA, Bradsher RW, Pappas PG, et al. (2008) Clinical practice guidelines for the management of blastomycosis: 2008 update by the Infectious Diseases Society of America. Clinical Infectious Diseases 46: 1801–1812
Larson DM, Eckman MR, Alber RL, Goldschmidt VG. Primary cutaneous (inoculation) blastomycosis: an occupational hazard to pathologist. Am J Clinc Pathol. 1983;79(2):253–255.
McBride, J. A., Gauthier, G. M., & Klein, B. S. (2017). Clinical Manifestations and Treatment of Blastomycosis. Clinics in chest medicine, 38(3), 435–449. doi:10.1016/j.ccm.2017.04.006
Saccente M, Woods GL. Clinical and laboratory update on blastomycosis. Clin Microbiol Rev. 2010
Smith JA, Riddell J, IV, Kauffman CA. Cutaneous manifestations of endemic mycoses. Curr Infect Dis Rep. 2013;15(5):440–449